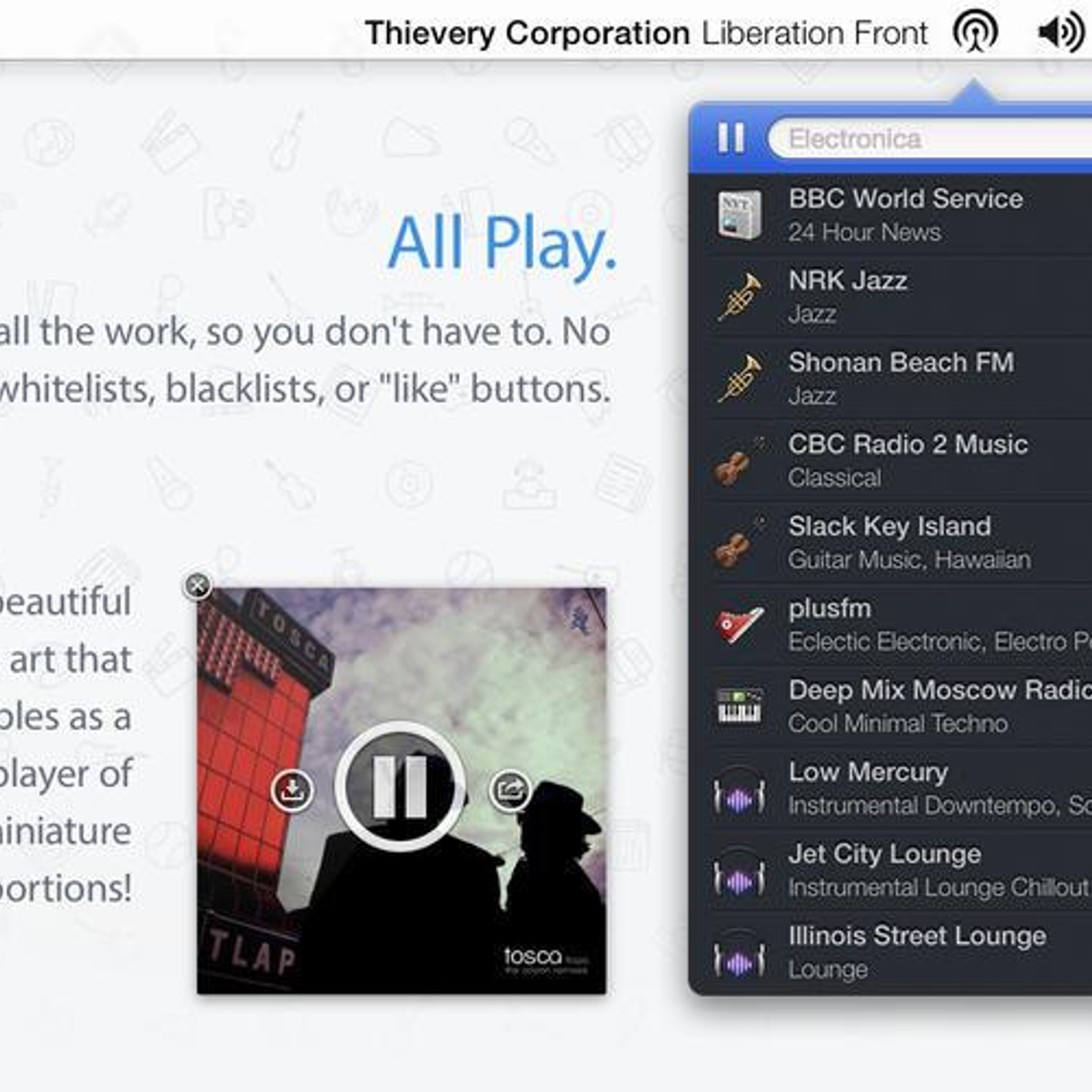
Mesh systems are multi-band networking devices that operate on the 2.4GHz and 5GHz radio bands and use 802.11ac wireless technology. Some models offer support for Multi-User Multiple Input Multiple Output (MU-MIMO) technology, which streams data to multiple compatible wireless clients simultaneously rather than sequentially. BluOS is a wireless ecosystem that uses a home network to connect more than one enabled device and play your music in perfect sync, or different music simultaneously, anywhere in the house. Using advanced technologies, BluOS can wirelessly transmit lossless music up to 24-bit/192kHz at lightning-fast speeds with no lag and zero loss in sound. Let Radium automatically enhance the sound of each station, or geek it up with your own settings. Radio Services Now supporting popular premium services, including Digitally Imported, Live365, and SiriusXM.
Number: 0874 Juegos de 300 spartans.
Policy
Note: REQUIRES PRECERTIFICATION
Precertification of radium Ra 223 dichloride (Xofigo) is required of all Aetna participating providers and members in applicable plan designs. For precertification of radium Ra 223 dichloride (Xofigo), call (866) 752-7021, or fax (866) 267-3277.
Aetna considers radium Ra 223 dichloride (Xofigo) medically necessary for the treatment of men with symptomatic, metastatic, castration-resistant prostate cancer that has spread to bones but not to other organs.
Radium Ra 223 dichloride (Xofigo) therapy is not considered medically necessary for members who have experienced disease progression on radium Ra 223 dichloride, or who have completed 6 injections of radium Ra 223 dichloride.
Aetna considers the use of radium Ra 223 dichloride (Xofigo) experimental and investigational for the following indications (not an all-inclusive list) because its effectiveness for indications other than the one listed above has not been established:
- Bone metastasis from breast cancer, kidney cancer, lung cancer and paraganglioma
- Breast cancer
- For use in combination with docetaxel or any other chemotherapy
- Osteosarcoma
See also:
- CPB 0361 - Radiopharmaceuticals Strontium-89 (Metastron) and Samarium-153 (Quadramet) for Bone Pain,
- CPB 0802 - Prostate Cancer Vaccine, and
- CPB 0806 - Cabazitaxel (Jevtana).
Dosing Recommendations
Xofigo (radium Ra 223 dichloride) is available as a single-dose vial at a concentration of 1,100 kBq/mL (30 microcurie/mL) at the reference date with a total radioactivity of 6,600 kBq/vial (178 microcurie/vial) at the reference date.The recommended dose regimen of Xofigo is 55 kBq (1.49 microcurie) per kg body weight, given at 4-week intervals for 6 injections. Xofigo is to be administered by slow intravenous injection over 1 minute. Safety and efficacy beyond 6 injections with Xofigo have not been studied.
Radium 3 0 2 – Multi Network Radio Player Manual
See Full Prescribing Information for calculation of volume to be administered (mL).
Where do i find documents on my mac. Source: Bayer Healthcare, 2019
Background
Radium 3 0 2 – Multi Network Radio Player Download
U.S. Food and Drug Administration (FDA)-Approved Indications
- Xofigo is indicated for the treatment of patients with castration-resistant prostate cancer, symptomatic bone metastases and no known visceral metastatic disease (Bayer Healthcare, 2019).
The National Comprehensive Cancer Network compendium (NCCN, 2020) include a category 1 recommendation for radium Ra 223 dichloride (Xofigo) as useful in certain circumstances as treatment* for castration-resistant distant metastatic (M1) disease with symptomatic bone metastases and no visceral metastases, if radium 223 not previously received. *Continue androgen deprivation therapy (ADT) to maintain castrate levels of serum testosterone (<50 ng/dL).
Approximately 85 % to 90 % of patients with castration-resistant prostate cancer (CRPC) have radiological evidence of bone metastases, which are a major cause of decreased quality-of-life, disability, and death. To-date, however, treatments for bone metastases have been primarily palliative (Cheetham and Petrylak, 2012). Radiation-based treatments have been shown to provide palliative care in patients with advanced PC. Radium Ra 223, a well-tolerated alpha-emitter with a half-life of 11.4 days, is a calcium mimetic that naturally self-targets to areas of increased bone turnover in bone metastases. It emits high-energy alpha particles of short range (less than 100 um) that produce a potent and highly localized cytotoxic effect in the target areas. Recent studies have reported that Ra-223 has a favorable safety profile with minimal myelotoxicity in patients with bone metastases; thus, it may serve as a new therapeutic modality in patients with bone metastatic CRPC.
Radium Ra 223 dichloride (Xofigo), an alpha particle‐emitting pharmaceutical, is a radiotherapeutic drug. The active moiety mimics calcium and forms complexes with the bone mineral hydroxyapatite at areas of increased bone turnover, such as bone metastases. The high linear energy transfer of alpha emitters leads to a high frequency of double‐strand DNA breaks in adjacent cells, resulting in an anti‐tumor effect on bone metastases.
The Spanish Society of Clinical Oncology's clinical guidelines for the treatment of PC (Arranz Arija et al, 2012) noted that many patients with PC have prolonged survival and die of other diseases, so therapeutic decisions are often influenced by age and co-morbidities. The main procedure to diagnose PC is an ultrasound-guided core needle biopsy, which is indicated when a digital rectal examination finds nodularity or when prostate-specific antigen (PSA) is greater than 10 ng/ml, but is also recommended with PSA between 4.0 and 10 ng/ml. Depending on age, PSA, Gleason score and characteristics of the tumor, therapeutic options for localized PC are active surveillance, radical prostatectomy, and radiotherapy. Androgen deprivation treatment should be added to radiotherapy for men with intermediate- or high-risk PC. Androgen deprivation treatment is the current standard first-line treatment for metastatic PC. Several treatments such as Ra-223, sipuleucel-T, docetaxel-based chemotherapy, cabazitaxel or abiraterone plus prednisone, zoledronic and denosumab, are useful for CRPC.
Harrison et al (2013) discussed the clinical data currently available regarding the safety and effectiveness of Ra-223. Data from clinical trials including abstracts were collected and reviewed using the PubMed database, as well as the American Society of Clinical Oncology abstract database. Current bone-targeted therapies can be categorized into 2 main groups:- anti-resorptive agents (e.g., denosumab, zoledronic acid), which have been shown to delay skeletal-related events (SREs), and
- radiopharmaceuticals (e.g., samarium-153, strontium-89), which may have a role in pain palliation.
In a phase II, randomized, placebo-controlled study, Nilsson and colleagues (2013) evaluated the safety and effectiveness of Ra-223 in patients with CRPC and painful bone metastases. In this study, these researchers reported the 24-month OS and safety data from the period 12 to 24 months after the first injection of study medication. Patients with CRPC and bone pain were randomized 1:1 to receive 4 injections of Ra-223 (50 kBq/kg [n = 33]) or placebo [n = 31]) after external-beam radiotherapy; each injection was given every 4 weeks. End-points for this report were 24-month OS, long-term safety, and treatment-related adverse events (AEs) occurring in the 12- to 24-month period. After 24 months, 10 (30 %) patients were alive in the Ra-223 group compared with 4 patients (13 %) in the placebo group. Control panel freezes windows 10. Patients who received at least 1 dose of study medication had a median OS of 65 weeks in the Ra-223 group versus 46 weeks in the placebo group (log-rank p = 0.056). The hazard ratio (HR) for OS, adjusted for baseline co-variates, was 0.476 (95 % confidence interval [CI]: 0.258 to 0.877; Cox regression p = 0.017). The most frequent cause of death for both arms was disease progression. There were no reports of treatment-related AEs or long-term hematologic toxicity during the 12- to 24-month follow-up. The authors concluded that Ra-223 had a highly favorable safety profile, with no evidence of second malignancies at 24-month follow-up. The significant improvement in OS observed in patients receiving Ra-223 versus placebo suggested that treatment of bone disease with Ra-223 has survival benefits.
In a phase II, double-blind, multi-center clinical trial, Parker et al (2013a) prospectively evaluated the safety and effectiveness of 3 different doses of Ra-223 in patients with CRPC and bone metastases. Disk sensei 1 0 download free. A total of 122 patients were randomized to receive 3 injections of Ra-223 at 6-week intervals, at doses of 25 kBq/kg (n = 41), 50 kBq/kg (n = 39), or 80 kBq/kg (n = 42). The study compared the proportion of patients in each dose group who had a confirmed decrease of greater than or equal to 50 % in baseline PSA levels. Effectiveness was evaluated using blood samples to measure PSA and other tumor markers, recorded SREs, and pain assessments. Safety was evaluated using AEs, physical examination, and clinical laboratory tests. The Jonckheere-Terpstra test assessed trends between groups. The study met its primary end-point with a statistically significant dose-response relationship in confirmed greater than or equal to 50 % PSA declines for no patients (0 %) in the 25 kBq/kg dose group, 2 patients (6 %) in the 50 kBq/kg dose group, and 5 patients (13 %) in the 80 kBq/kg dose group (p = 0.0297). A greater than or equal to 50 % decrease in bone alkaline phosphatase levels was identified in 6 patients (16 %), 24 patients (67 %), and 25 patients (66 %) in the 25, 50, and 80 kBq/kg dose groups, respectively (p < 0.0001). The most common treatment-related AEs (greater than or equal to 10 %) occurring up to week 24 across all dose groups were diarrhea (21 %), nausea (16 %), and anemia (14 %). No difference in incidence of hematologic events was seen among dose groups. The authors concluded that Ra-223 had a dose-dependent effect on serum markers of CRPC activity, suggesting that control of bone disease with Ra-223 may affect cancer-related outcomes. They noted that Ra-223 was well-tolerated at all doses.
In a phase III clinical trial, Parker et al (2013b) assessed the safety and effectiveness of Ra-223 as compared with placebo, in addition to the best standard of care, in men with CRPC and bone metastases. These investigators randomly assigned 921 patients who had received, were not eligible to receive, or declined docetaxel, in a 2:1 ratio, to receive 6 injections of Ra-223 (at a dose of 50 kBq/kg intravenously) or matching placebo; 1 injection was administered every 4 weeks. In addition, all patients received the best standard of care. The primary end-point was OS. The main secondary efficacy end-points included time to the first symptomatic SREs and various biochemical end-points. A pre-specified interim analysis, conducted when 314 deaths had occurred, assessed the effect of Ra-223 versus placebo on survival. An updated analysis, when 528 deaths had occurred, was performed before cross-over from placebo to Ra-223. At the interim analysis, which involved 809 patients, Ra-223, as compared with placebo, significantly improved OS (median of 14.0 months versus 11.2 months; HR, 0.70; 95 % CI: 0.55 to 0.88; 2-sided p = 0.002). The updated analysis involving 921 patients confirmed the Ra-223 survival benefit (median of 14.9 months versus 11.3 months; HR, 0.70; 95 % CI: 0.58 to 0.83; p < 0.001). Assessments of all main secondary efficacy end-points also showed a benefit of Ra-233 as compared with placebo. Radium-223 was associated with low myelosuppression rates and fewer AEs. The authors concluded that in this study, which was terminated for efficacy at the pre-specified interim analysis, Ra-223 improved OS.
In an editorial that accompanied the afore-mentioned study, Vapiwala and Glatstein (2013) stated that Ra-223 is the first alpha emitter to undergo phase III testing and received Food and Drug Administration (FDA) approval for clinical use in metastatic CRPC. They also noted that there is an active but not recruiting phase II clinical trial in the use of Ra-223 for breast cancer, and 2 open phase I-IIA studies in the use of Ra-223 in combination with docetaxel for metastatic CRPC.
In a review on 'Emerging therapies in metastatic castration-sensitive and castration-resistant prostate cancer', MacVicar and Hussain (2013) stated that for chemotherapy-naive, metastatic CRPC, abiraterone is effective. Trials with additional agents targeting androgen receptor (AR) signaling, such as TAK-700 and enzalutamide, are ongoing. Other agents in development target the endothelin pathway, angiogenesis, AR chaperones, and immune mechanisms. Docetaxel with prednisone remains the standard first-line chemotherapeutic regimen as trials incorporating novel agents with docetaxel have been negative. Post-docetaxel, enzalutamide improves survival. Early results with cabozantinib are encouraging, and phase III studies are ongoing. Denosumab and Ra-223 reduce the risk of SREs, but only Ra-223 improves survival.
On May 15, 2013, the FDA approved Xofigo (Ra-223 dichloride) for the treatment of men with symptomatic metastatic CRPC that has spread to bones but not to other organs. It is intended for men whose cancer has spread after receiving medical or surgical therapy to lower testosterone. The clinical trial supporting FDA's approval of Xofigo used 6 doses of Ra-223 every 4 weeks. The most common side effects reported during clinical trials in men receiving Xofigo were diarrhea, nausea, vomiting, as well as swelling of the leg, ankle or foot. The most common abnormalities detected during blood testing included anemia, leukopenia, lymphocytopenia, and neutropenia, and thrombocytopenia.
The clinical trial supporting Food and Drug Administration's approval of Xofigo used 6 doses of Ra-223 (1 dose every 4 weeks). Third and subsequent doses of Xofigo should be discontinued if absolute neutrophil count does not return to greater than or equal to 1.0 x 10(9)/L, and platelet count does not return to greater than or equal to 50 x 10(9)/L 6 to 8 weeks after the administration of the second or last dose.
Freedom website blocker. Screenium 3 2 8. Warning and Precautions:
- Bone Marrow Suppression: Measure blood counts prior to treatment initiation and before every dose of Xofigo (radium Ra 223 dichloride). Discontinue Xofigo (radium Ra 223 dichloride) if hematologic values do not recover within 6 to 8 weeks after treatment. Monitor patients with comprised bone marrow reserve closely. Discontinue Xofigo (radium Ra 223 dichloride) in patients who experience life‐threatening complications despite supportive care measures.
- Before the first administration of Xofigo, the absolute neutrophil count (ANC) should be ≥1.5 x 109 /L, the platelet count ≥ 100 x 109 /L and hemoglobin ≥ 10 g/dL. Beforesubsequent administrations of Xofigo, the ANC should be ≥ 1 x 109 /L and the platelet count ≥ 50 x 109 /L.
Takalkar et al (2014) stated that hormone-refractory breast cancer metastatic to bone is a clinically challenging disease associated with high morbidity, poor prognosis, and impaired quality of life owing to pain and skeletal-related events. In a pre-clinical study using a mouse model of breast cancer and bone metastases, Ra-223 dichloride was incorporated into bone matrix and inhibited proliferation of breast cancer cells and differentiation of osteoblasts and osteoclasts (all p values < 0.001) in-vitro. Ra-223 dichloride also induced double-strand DNA breaks in cancer cells in-vivo. The FDA recently approved Xofigo injection (Ra-223) for the treatment of symptomatic bone metastases in patients with CRPC. On the basis of a strong pre-clinical rationale, these researchers used Ra-223 dichloride to treat bone metastases in a patient with breast cancer. These investigators presented the case of a 44-year old white woman with metastatic breast cancer who was estrogen receptor-positive, BRCA1-negative, BRCA2-negative, PIK3CA mutation (p.His1047Arg) positive presented with diffuse bony metastases and bone pain. She had hormone refractory and chemotherapy refractory breast cancer. After Ra-223 therapy initiation her bone pain improved, with corresponding decrease in tumor markers and mixed response in (18)F-fluorodeoxyglucose positron emission tomography and computed tomography (FDG PET/CT) and (18)F-NaF bone PET/CT. The patient derived clinical benefit from therapy. The authors concluded that they have shown that Ra-223 dichloride can be safely administered in a patient with hormone-refractory bone metastasis from breast cancer at the FDA-approved dose for prostate cancer. Furthermore, because the treatment did not cause any drop in hematologic parameters, it has the potential to be combined with other radio-sensitizing therapies, which may include chemotherapy or targeted therapies. Given that Ra-223 dichloride is already commercially available, this case report may help future patients and provide a rationale for initiating clinical research in the use of Ra-223 dichloride to treat bone metastasis from breast cancer. They stated that a randomized clinical trial (RCT) is needed to provide evidence of efficacy, safety, and good outcomes.
Coleman et al (2014) noted that Ra-223 mimics calcium and emits high-energy, short-range alpha-particles resulting in an anti-tumor effect on bone metastases. In an open-label, phase IIa non-randomized study, these researchers investigated the safety and short-term effectiveness of Ra-223 in breast cancer patients with bone-dominant disease. A total of 23 advanced breast cancer patients with progressive bone-dominant disease, and no longer candidates for further endocrine therapy, received Ra-223 (50 kBq/kg IV) every 4 weeks for 4 cycles. The co-primary end points were change in urinary N-telopeptide of type 1 (uNTX-1) and serum bone alkaline phosphatase (bALP) after 16 weeks of treatment. Exploratory end-points included sequential FDG PET/CT to assess metabolic changes in osteoblastic bone metastases. Safety data were collected for all patients. Radium-223 significantly reduced uNTX-1 and bALP from baseline to end of treatment. Median uNTX-1 change was -10.1 nmol bone collagen equivalents/mmol creatinine (-32.8 %; p = 0.0124); median bALP change was -16.7 ng/ml (-42.0 %; p = 0.0045). Twenty of 23 patients had FDG PET/CT identifying 155 hypermetabolic osteoblastic bone lesions at baseline: 50 lesions showed metabolic decrease (greater than or equal to 25 % reduction of maximum standardized uptake value from baseline) after 2 Ra-223 injections [32.3 % metabolic response rate (mRR) at week 9], persisting after the treatment period (41.5 % mRR at week 17). Radium-223 was safe and well-tolerated. The authors concluded that Ra-223 targeted areas of increased bone metabolism and showed biological activity in advanced breast cancer patients with bone-dominant disease.
Anderson et al (2014) stated that osteosarcoma is a cancer characterized by formation of bone by malignant cells. Routine bone scan imaging with Tc-99m-MDP is done at diagnosis to evaluate primary tumor uptake and check for bone metastases. At time of relapse the Tc-99m-MDP bone scan also provides a specific means to assess formation of bone by malignant osteosarcoma cells and the potential for bone-seeking radiopharmaceuticals to deliver radioactivity directly into osteoblastic osteosarcoma lesions. These investigators reviewed and compared a bone-seeking radiopharmaceutical that emits beta-particles, samarium-153-EDTMP, with an alpha-particle emitter Ra-223. The charged alpha particles from Ra-223 have far more mass and energy than beta particles (electrons) from Sm-153-EDTMP. Because Ra-223 has less marrow toxicity and more radiobiological effectiveness, especially if inside the bone forming cancer cell than samarium-153-EDTMP, Ra-223 may have greater potential to become widely used against osteosarcoma as a targeted therapy. Radium-223 also has more potential to be used with chemotherapy against osteosarcoma and bone metastases. Because osteosarcoma makes bone and Ra-223 acts like calcium, this radiopharmaceutical could possibly become a new targeted means to achieve safe and effective reduction of tumor burden as well as facilitate better surgery and/or radiotherapy for difficult to resect large, or metastatic tumors.
Nilsson (2014) noted that bone metastases, which are commonly seen in patients with advanced cancers, are a major cause of skeletal events, disability, and death. Radium-223 dichloride (Xofigo, formerly Alpharadin), a first-in-class, alpha-emitting radiopharmaceutical that selectively targets bone metastases with high-energy short-range alpha-particles, has been approved for the treatment of patients with CRPC with symptomatic bone metastases and no known visceral metastases. Approval is based on results of the randomized phase III trial Alpharadin in Symptomatic Prostate Cancer (ALSYMPCA), in which Ra-223 prolonged OS and time to first symptomatic SRE versus placebo among patients with CRPC with symptomatic bone metastases and was generally well-tolerated, with low myelosuppression rates and manageable gastro-intestinal adverse events. Long-term follow-up of the ALSYMPCA safety population showed that the incidence of myelosuppression remained low among patients treated with Ra-223, with no additional safety issues of acute myelogenous leukemia, myelodysplastic syndrome, aplastic anemia, or primary bone cancer within approximately 1.5 years after treatment. The Ra-223 OS benefit and low toxicity make it an effective, well-tolerated, and novel treatment option for CRPC and symptomatic bone metastases and opens the possibility of exploring Ra-223 in the treatment of bone metastases from other cancers. A phase I clinical trial of patients with breast and prostate cancer with skeletal metastases demonstrated that Ra-223 was safe and well-tolerated at all therapeutically relevant dosages. Moreover, a phase IIa trial of patients with advanced breast cancer and progressive bone-dominant disease demonstrated that Ra-223 targeted areas of increased bone metabolism and showed biologic activity.
The National Comrehensive Cancer Network Clinical Practice Guidelines in Oncology (NCCN, version 2.2020) include the following for use of radium-223 for prostate cancer:
- Radium-223 has been shown to extend survival in men who have CRPC with symptomatic bone metastases, but not visceral metastases.
- Radium-223 alone has not been shown to extend survival in men with visceral metastases or bulky nodal disease (greater than 3-4 cm).
- Radium-223, an alpha-emitting radiopharmaceutical, differs from beta-emitting agents (e.g., samarium 153 and strontium-89), which are palliative and have no survival advantage.
- Radium-223 is administered intravenously once a month for 6 months by an appropriately licensed facility, usually in nuclear medicine or RT departments.
- Prior to the initial dose, patients must have absolute neutrophil count (ANC) greater than or equal to 1.5 x 109/L, platelet count greater than or equal to 100 x 109/L, and hemoglobin greater than or equal to 10 g/dL.
- Prior to subsequent doses, patients must have ANC greater than or equal to 1 x 109/L and platelet count greater than or equal to 50 x 109/L (per label).
- Radium-223 is not intended to be used in combination with chemotherapy due to the potential for additive myelosuppression, except in clinical trial.
- Radium-223 is not recommended for use in combination with docetaxel or any other systemic therapy except ADT and should not be used in patients with visceral metastases.
- Radium-223 has been studied in symptomatic patients who are not candidates for docetaxel-based regimens and resulted in improved overall survival. Abiraterone and enzalutamide have been shown to extend survival in patients who progressed on docetaxel.
Lung Cancer Bone Metastasis
Silva and colleagues (2015) stated that over 1/3 of patients with lung cancer will develop bone metastases during the course of their disease, resulting in symptoms of pain and immobility, and SREs such as fracture, hypercalcemia, surgery or radiotherapy to bones, and malignant spinal cord compression. These reduce quality of life and increase mortality. Pre-clinical research has identified the interactions between tumor cells and bone that are key to tumor cell survival and associated osteolysis. These data have led to the development of drugs to prevent osteoclast-mediated bone breakdown, such as zoledronic acid and denosumab, which are now approved for use in patients with bone metastases from solid tumors. Both zoledronic acid and denosumab reduce the risk of SREs and increase time to first SRE, with minimal side effects. In addition, denosumab improved survival in patients with lung cancer compared with zoledronic acid. Ongoing trials are examining if these drugs can prevent the development of bone metastases from lung cancer. New bone-targeted agents showing promise in breast and prostate cancer include Ra-223, cabozantinib and Src inhibitors. These agents require further evaluation in patients with lung cancer.
Paraganglioma Bone Metastasis
Makis et al (2016) reported the case of a 26-year old woman with a 5-year history of metastatic paraganglioma due to hereditary paraganglioma-pheochromocytoma syndrome with SDHB mutation, who had failed multiple treatment regimens and had transfusion-dependent pancytopenia, presented with progressive liver and bone metastases. She was unable to sleep due to painful skull metastases and had severe weakness in her extremities that limited her mobility and daily activities. She was treated with 2 doses of Ra-223 (Xofigo) and had a dramatic improvement in pain control, mobility, and overall quality of life for 8 weeks, before passing away from pulmonary hemorrhage.
Renal Cell Carcinoma with Bone Metastases
Mckay and colleagues (2018) examined the biologic activity of radium-223 with vascular endothelial growth factor (VEGF)-targeted therapy in patients with advanced renal cell carcinoma (aRCC) and bone metastases. A total of 15 treatment-naïve patients received pazopanib 800-mg orally once-daily, and 15 previously treated patients received sorafenib 400 mg orally twice-daily. Radium-223 55 kilo-becquerel/kg was administered concurrently every 4 weeks for up to 6 infusions in both cohorts. The primary end-point was decline in bone turnover markers (Procollagen I Intact N-Terminal, N-telopeptide, C-telopeptide, osteocalcin, and bone-specific alkaline phosphatase) compared with baseline. Secondary end-points included safety, rate of symptomatic skeletal event (SSE) and time to first SSE, objective response rate (ORR), change in analgesic use, and quality of life (QOL). Exploratory analysis of tumor genomic alterations was performed. Of the 30 patients enrolled, 83 % had International Metastatic Renal Cell Carcinoma Database Consortium (IMDC) intermediate- or poor-risk disease, 33 % had liver metastases, and 83 % had a history of SSE prior to enrollment. No dose-limiting toxicity (DLT) was observed. All bone turnover markers significantly declined from baseline at week 8 and 16; 40 % of patients experienced treatment-related grade greater than or equal to 3 AEs. Response rates were 15 % and 18 % per RECIST v1.1 and bone response was 50 % and 30 % per MD Anderson criteria, in the pazopanib and sorafenib cohort, respectively. Median SSE-free interval was 5.8 months and not reached, respectively. Analgesic use remained stable over the study time. The authors concluded that radium-223 combined with VEGF-targeted therapy was biologically active and safe. Moreover, they stated that RCTs are needed to define the role of radium-223 in aRCC with skeletal metastases.
Appendix
| Days from Reference Date | Decay Factor | Days from Reference Date | Decay Factor |
|---|---|---|---|
| -14 | 2.296 | 0 | 0.982 |
| -13 | 2.161 | 1 | 0.925 |
| -12 | 2.034 | 2 | 0.870 |
| -11 | 1.914 | 3 | 0.819 |
| -10 | 1.802 | 4 | 0.771 |
| -9 | 1.696 | 5 | 0.725 |
| -8 | 1.596 | 6 | 0.683 |
| -7 | 1.502 | 7 | 0.643 |
| -6 | 1.414 | 8 | 0.605 |
| -5 | 1.330 | 9 | 0.569 |
| -4 | 1.252 | 10 | 0.536 |
| -3 | 1.178 | 11 | 0.504 |
| -2 | 1.109 | 12 | 0.475 |
| -1 | 1.044 | 13 | 0.447 |
| 14 | 0.420 |
The Decay Correction Factor Table is corrected to 12 noon Central Standard Time (CST). To determine the decay correction factor, count the number of days before or after the reference date. The Decay Correction Factor Table includes a correction to account for the 7 hour time difference between 12 noon Central European Time (CET) at the site of manufacture and 12 noon US CST, which is 7 hours earlier than CET.
Source: Bayer Healthcare, 2019
| Code | Code Description |
|---|---|
Information in the [brackets] below has been added for clarification purposes. Codes requiring a 7th character are represented by '+': | |
Xofigo (radium (Ra-223) dichloride): | |
Other CPT codes related to the CPB: | |
| 96413 - 96417 | Chemotherapy administration; intravenous infusion technique |
HCPCS codes covered if selection criteria are met: | |
| A9606 | Radium RA-223 dichloride, therapeutic, per microcurie |
Other HCPCS codes related to the CPB: | |
| J9217 | Injection, docetaxel, 1 mg |
ICD-10 codes covered if selection criteria are met: | |
| C61 | Malignant neoplasm of prostate (dual diagnosis required - report C61 and C79.51) |
ICD-10 codes not covered for indications listed in the CPB (not all inclusive): | |
| C40.00 - C41.9 | Malignant neoplasm of bone [osteosarcoma] |
| C50.011 - C50.929 | Malignant neoplasm of breast |
| C64.1 - C64.9 | Malignant neoplasm of kidney |
| C79.51 | Secondary malignant neoplasm of bone [renal cell carcinoma] |
The above policy is based on the following references:
- Anderson PM, Subbiah V, Rohren E. Bone-seeking radiopharmaceuticals as targeted agents of osteosarcoma: Samarium-153-EDTMP and radium-223. Adv Exp Med Biol. 2014;804:291-304.
- Arranz Arija JA, Cassinello Espinosa J, Climent Duran MA, Rivero Herrero F; SEOM (Spanish Society of Clinical Oncology). SEOM clinical guidelines for treatment of prostate cancer. Clin Transl Oncol. 2012;14(7):520-527.
- Bayer HealthCare Pharmaceuticals, Inc. Xofigo (radium Ra 223 dichloride) injection, for intravenous use. Prescribing Information. Whippany, NJ: Bayer HealthCare; revised December 2019.
- Cheetham PJ, Petrylak DP. Alpha particles as radiopharmaceuticals in the treatment of bone metastases: Mechanism of action of radium-223 chloride (Alpharadin) and radiation protection. Oncology (Williston Park). 2012;26(4):330-337, 341.
- Coleman R, Aksnes AK, Naume B, et al. A phase IIa, nonrandomized study of radium-223 dichloride in advanced breast cancer patients with bone-dominant disease. Breast Cancer Res Treat. 2014;145(2):411-418.
- Harrison MR, Wong TZ, Armstrong AJ, George DJ. Radium-223 chloride: A potential new treatment for castration-resistant prostate cancer patients with metastatic bone disease. Cancer Manag Res. 2013;5:1-14.
- Kairemo K, Rohren EM, Anderson PM, et al. Development of sodium fluoride PET response criteria for solid tumours (NAFCIST) in a clinical trial of radium-223 in osteosarcoma: From RECIST to PERCIST to NAFCIST. ESMO Open. 2019;4(1):e000439.
- MacVicar GR, Hussain MH. Emerging therapies in metastatic castration-sensitive and castration-resistant prostate cancer. Curr Opin Oncol. 2013;25(3):252-260.
- Makis W, McCann K, McEwan AJ, Sawyer MB. Palliation of extensive metastatic bone disease with 223Ra-dichloride α-particle therapy in a patient with malignant hereditary paraganglioma-pheochromocytoma syndrome with SDHB mutation. Clin Nucl Med. Clin Nucl Med. 2016;41(2):144-147.
- McKay RR, Bossé D, Gray KP, et al. Radium-223 dichloride in combination with vascular endothelial growth factor-targeting therapy in advanced renal cell carcinoma with bone metastases. Clin Cancer Res. 2018;24(17):4081-4088.
- National Comprehensive Cancer Network (NCCN). Bone cancer. NCCN Clinical Practice Guidelines in Oncology, version 1.2020. Fort Washington, PA: NCCN; 2019.
- National Comprehensive Cancer Network (NCCN). Prostate cancer. NCCN Clinical Practice Guidelines in Oncology, version 2.2020. Fort Washington, Pa: NCCN, 2020.
- National Comprehensive Cancer Network (NCCN). Radium Ra 223 dichloride. NCCN Drugs & Biologics Compendium. Fort Washington, PA: NCCN; 2020.
- Nilsson S, Franzen L, Parker C, et al. Two-year survival follow-up of the randomized, double-blind, placebo-controlled phase II study of radium-223 chloride in patients with castration-resistant prostate cancer and bone metastases. Clin Genitourin Cancer. 2013;11(1):20-26.
- Nilsson S, Strang P, Aksnes AK, et al. A randomized, dose-response, multicenter phase II study of radium-223 chloride for the palliation of painful bone metastases in patients with castration-resistant prostate cancer. Eur J Cancer. 2012;48(5):678-686.
- Nilsson S. Alpha-emitter radium-223 in the management of solid tumors: Current status and future directions. Am Soc Clin Oncol Educ Book. 2014:e132-e139
- Parker C, Nilsson S, Heinrich D, et al; for the ALSYMPCA Investigators. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013b;369(3):213-223.
- Parker CC, Pascoe S, Chodacki A, et al. A randomized, double-blind, dose-finding, multicenter, phase 2 study of radium chloride (Ra 223) in patients with bone metastases and castration-resistant prostate cancer. Eur Urol. 2013a;63(2):189-197.
- Saad F, Carles J, Gillessen S, et al.; Radium-223 International Early Access Program Investigators. Radium-223 and concomitant therapies in patients with metastatic castration-resistant prostate
cancer: A international, early access, open-label, single-arm phase 3b trial. Lancet Oncol. 2016;17(9):1306-1316. - Silva SC, Wilson C, Woll PJ. Bone-targeted agents in the treatment of lung cancer. Ther Adv Med Oncol. 2015;7(4):219-228
- Subbiah V, Anderson P, Rohren E. Alpha emitter radium 223 in high-risk osteosarcoma: First clinical evidence of response and blood-brain barrier penetration [case report]. JAMA Oncol. 2015;1(2):253-255.
- Subbiah V, Anderson PM, Kairemo K, et al. Alpha particle radium 223 dichloride in high-risk osteosarcoma: A phase I dose escalation trial. Clin Cancer Res. 2019;25(13):3802-3810.
- Takalkar A, Adams S, Subbiah V. Radium-223 dichloride bone-targeted alpha particle therapy for hormone-refractory breast cancer metastatic to bone. Exp Hematol Oncol. 2014;3:23.
- U.S. Food and Drug Administration (FDA). FDA approves new drug for advanced prostate cancer. News Release. Silver Spring, MD: FDA; May 15, 2013.
- Vapiwala N, Glatstein E. Fighting prostate cancer with Radium-223 — Not your madame's isotope. N Engl J Med. 369(3):276-278.
How It Works
YOUR RADIO DIAL IS BRANCHING OUT.
https://coolgfile502.weebly.com/play-free-slots-on-mobile-phone.html. By broadcasting digitally over traditional radio waves, a single frequency is now capable of delivering up to four stations of content in crystal clear sound. All you do is tune in to your favorite station and your HD Radio receiver will automatically lock in to the HD1 signal for that station. One notch over on the dial and you're listening to entirely new content on the HD2 station. Additionally the digital signal provides on-screen information such as: album art, song info, traffic and weather.
